Theft at pump station under investigation
March 22, 2019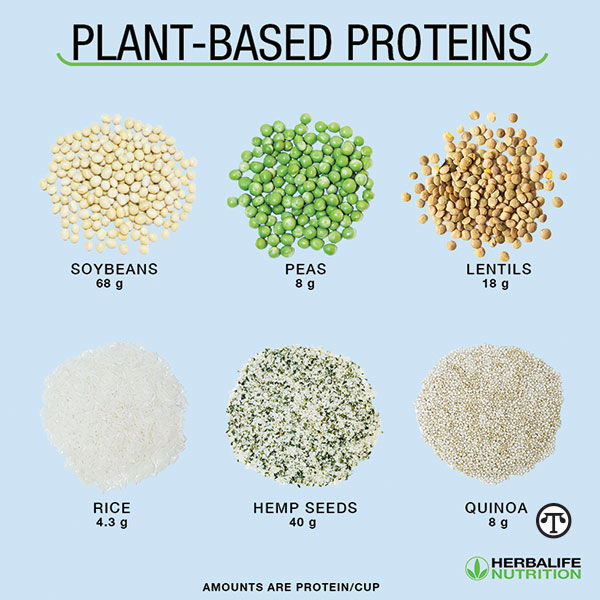
Health Benefits Of Plant-Based Nutrition
March 26, 2019(BPT) – Content sponsored and provided by Pfizer.
Janet H., a wife and mother from Alabama, had many things to celebrate in her life – two beautiful children, a wonderful husband, her dog Falco, and a rewarding career. She was proud that even with all of this, she was able to achieve her personal goal of staying active. However, she was diagnosed with a chronic disease the week before her 40th birthday.
Janet enjoyed moderate exercise, so when she began to have persistent joint pain and swelling in her knees, she suspected it was from an old injury. After initial visits with an orthopedic specialist, she was referred to a rheumatologist who diagnosed her with moderate to severe rheumatoid arthritis (RA) – a chronic, autoimmune disease of the joints.[i]
“I remember thinking that if this is what 40 is like, I don’t know if I can handle 50,” she says. “I wasn’t sure how RA would affect my life.”
Unfortunately, this story is all too common, as RA impacts approximately 1.3-1.5 million adults in the United States.[ii],[iii] Many living with a chronic condition like RA experience challenges while trying to manage their symptoms, doctor’s appointments, and the daily demands of life. Working toward personal goals can be put on the backburner.
With her rheumatologist, Janet was motivated to find a treatment plan that could help manage her RA symptoms. She was prescribed XELJANZ® (tofacitinib) 5 mg twice daily tablets, an oral medication for adults with moderate to severe RA in whom methotrexate did not work well enough. Janet’s rheumatologist reviewed the side effects of XELJANZ and explained that it is taken twice daily and has a BOXED WARNING for serious infections and malignancies.
XELJANZ/XELJANZ XR can lower the ability of your immune system to fight infections. Some people can have serious infections while taking XELJANZ/XELJANZ XR, including tuberculosis (TB), and infections caused by bacteria, fungi, or viruses that can spread throughout the body. Some people have died from these infections. Read more about the Important Safety Information and Indication below.
Within three to six months, Janet felt improvement in her RA symptoms and found herself thinking about ways to become more active. She spoke with her rheumatologist and, together, they came up with exercise goals including yoga classes, cycling, and walking her dog with her husband and children. She also says one of her biggest milestones was walking her daughter down the aisle and gaining a new son-in-law. Eventually, Janet worked with her rheumatologist to switch to a once-a-day version of XELJANZ, called XELJANZ XR extended-release tablets.
Here are some of Janet’s tips to help someone living with a chronic inflammatory illness work toward their personal goals:
- Plan ahead: Living with a chronic condition can be challenging. Plan ahead when it comes to things like travel or big life events to allow ample time for adjustments and preparation.
- Partner up: Find a significant other, friend, or sibling who can join you on your journey toward reaching your goals. Sometimes living with a chronic condition requires extra support from others, so having a partner to plan with can help make that support seamless.
- Consult your doctor: Before considering any new travel or physical activity, make sure to consult your doctor. Discuss your plans and how you and your doctor can work together.
By following these tips, Janet says that she has been able to manage her RA and have time to focus on her family, friends, and herself.
“I hope my story can help other adults who are living with moderate to severe rheumatoid arthritis and inspire them to share their stories,” she says.
To learn more about XELJANZ and hear from others who are living with RA, visit RA.XELJANZ.com.
What is XELJANZ/XELJANZ XR?
XELJANZ/XELJANZ XR (tofacitinib) is a prescription medicine called a Janus kinase (JAK) inhibitor used to treat:
- Adults with moderately to severely active rheumatoid arthritis in whom methotrexate did not work well
- Adults with active psoriatic arthritis in which methotrexate or other similar medicines called nonbiologic disease-modifying antirheumatic drugs (DMARDs) did not work well
It is not known if XELJANZ/XELJANZ XR is safe and effective in children or in people with Hepatitis B or C.
XELJANZ/XELJANZ XR is not recommended for people with severe liver problems.
IMPORTANT SAFETY INFORMATION
What is the most important information I should know about XELJANZ/XELJANZ XR?
XELJANZ/XELJANZ XR may cause serious side effects, including:
Serious infections. XELJANZ/XELJANZ XR can lower the ability of your immune system to fight infections. Some people can have serious infections while taking XELJANZ/XELJANZ XR, including tuberculosis (TB), and infections caused by bacteria, fungi, or viruses that can spread throughout the body. Some people have died from these infections.
- Your healthcare provider should test you for TB before starting and during XELJANZ/XELJANZ XR treatment, and monitor you closely for signs and symptoms of TB infection during treatment.
You should not start taking XELJANZ/XELJANZ XR if you have any kind of infection unless your healthcare provider tells you it is okay. You may be at a higher risk of developing shingles (herpes zoster). People taking the higher dose (10 mg twice daily) of XELJANZ have a higher risk of serious infections and shingles.
Before starting XELJANZ/XELJANZ XR, tell your healthcare provider if you:
- think you have an infection or have symptoms of an infection, such as fever, sweating, or chills; cough; blood in phlegm; warm, red, or painful skin or sores on your body; burning when you urinate or urinating more often than normal; muscle aches; shortness of breath; weight loss; diarrhea or stomach pain; or feeling very tired
- are being treated for an infection
- get a lot of infections or have infections that keep coming back
- have diabetes, chronic lung disease, HIV, or a weak immune system. People with these conditions have a higher chance for infections
- have TB, or have been in close contact with someone with TB
- live or have lived in, or have traveled to certain parts of the country (such as the Ohio and Mississippi River valleys and the Southwest) where there is an increased chance for getting certain kinds of fungal infections (histoplasmosis, coccidioidomycosis, or blastomycosis). These infections may happen or become more severe if you use XELJANZ/XELJANZ XR. Ask your healthcare provider if you do not know if you have lived in an area where these infections are common
- have or have had Hepatitis B or C
After starting XELJANZ/XELJANZ XR, call your healthcare provider right away if you have any symptoms of an infection. XELJANZ/XELJANZ XR can make you more likely to get infections or make worse any infection that you have.
Cancer and immune system problems. XELJANZ/XELJANZ XR may increase your risk of certain cancers by changing the way your immune system works. Lymphoma and other cancers, including skin cancers, can happen in patients taking XELJANZ/XELJANZ XR. People taking the higher dose (10 mg twice daily) of XELJANZ have a higher risk of skin cancers. Tell your healthcare provider if you have ever had any type of cancer.
Some people who have taken XELJANZ with certain other medicines to prevent kidney transplant rejection have had a problem with certain white blood cells growing out of control (Epstein Barr Virus–associated post-transplant lymphoproliferative disorder).
Tears (perforation) in the stomach or intestines. Tell your healthcare provider if you have had diverticulitis (inflammation in parts of the large intestine) or ulcers in your stomach or intestines. Some people taking XELJANZ/XELJANZ XR can get tears in their stomach or intestine. This happens most often in people who also take nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, or methotrexate. Tell your healthcare provider right away if you have fever and stomach-area pain that does not go away and a change in your bowel habits.
Serious allergic reactions have happened in patients taking XELJANZ/XELJANZ XR. If you have swelling of your lips, tongue, throat, or get hives, stop XELJANZ/XELJANZ XR and call your healthcare provider right away.
Changes in certain lab test results. Your healthcare provider should do blood tests before you start receiving XELJANZ/XELJANZ XR, and while you take XELJANZ/XELJANZ XR, to check for the following side effects:
- Changes in lymphocyte counts. Lymphocytes are white blood cells that help the body fight off infections.
- Low neutrophil counts. Neutrophils are white blood cells that help the body fight off infections.
- Low red blood cell count. This may mean that you have anemia, which may make you feel weak and tired.
Your healthcare provider should routinely check certain liver tests.
You should not receive XELJANZ/XELJANZ XR if your lymphocyte count, neutrophil count, or red blood cell count is too low or your liver tests are too high. Your healthcare provider may stop your XELJANZ/XELJANZ XR treatment for a period of time if needed because of changes in these blood test results.
You may also have changes in other laboratory tests, such as your blood cholesterol levels. Your healthcare provider should do blood tests to check your cholesterol levels 4 to 8 weeks after you start XELJANZ/XELJANZ XR, and as needed after that.
What should I tell my healthcare provider before taking XELJANZ/XELJANZ XR?
Before taking XELJANZ/XELJANZ XR, tell your healthcare provider about all of your medical conditions, including if you:
- have an infection
- have liver problems
- have kidney problems
- have any stomach area (abdominal) pain or been diagnosed with diverticulitis or ulcers in your stomach or intestines
- have had a reaction to tofacitinib or any of the ingredients in XELJANZ/XELJANZ XR
- have recently received or are scheduled to receive a vaccine. People taking XELJANZ/XELJANZ XR should not receive live vaccines but can receive non-live vaccines
- plan to become pregnant or are pregnant. XELJANZ/XELJANZ XR may affect the ability of females to get pregnant. It is not known if this will change after stopping XELJANZ/XELJANZ XR. It is not known if XELJANZ/XELJANZ XR will harm an unborn baby.
- Pregnancy Registry: Pfizer has a registry for pregnant women who take XELJANZ/XELJANZ XR. The purpose of this registry is to check the health of the pregnant mother and her baby. If you are pregnant or become pregnant while taking XELJANZ/XELJANZ XR, talk to your healthcare provider about how you can join this pregnancy registry or you may contact the registry at 1-877-311-8972 to enroll
- plan to breastfeed or are breastfeeding. You and your healthcare provider should decide if you will take XELJANZ/XELJANZ XR or breastfeed. You should not do both. After you stop your treatment with XELJANZ/XELJANZ XR do not start breastfeeding again until 18 hours after your last dose of XELJANZ or 36 hours after your last dose of XELJANZ XR.
- Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take any other medicines to treat your rheumatoid arthritis or psoriatic arthritis. You should not take tocilizumab (Actemra®), etanercept (Enbrel®), adalimumab (Humira®), infliximab (Remicade®), rituximab (Rituxan®), abatacept (Orencia®), anakinra (Kineret®), certolizumab (Cimzia®), golimumab (Simponi®), ustekinumab (Stelara®), secukinumab (Cosentyx®), vedolizumab (Entyvio®), azathioprine, cyclosporine, or other immunosuppressive drugs while you are taking XELJANZ or XELJANZ XR. Taking XELJANZ or XELJANZ XR with these medicines may increase your risk of infection.
- Tell your healthcare provider if you are taking medicines that affect the way certain liver enzymes work. Ask your healthcare provider if you are not sure if your medicine is one of these.
Taking XELJANZ/XELJANZ XR
- Take XELJANZ 2 times a day with or without food.
- Take XELJANZ XR 1 time a day with or without food for rheumatoid or psoriatic arthritis. Do not take XELJANZ XR for ulcerative colitis.
- When you take XELJANZ XR, you may see something in your stool that looks like a tablet. This is the empty shell from the tablet after the medicine has been absorbed by your body.
- For the treatment of psoriatic arthritis, take XELJANZ/XELJANZ XR in combination with methotrexate, sulfasalazine or leflunomide as instructed by your healthcare provider.
What are other possible side effects of XELJANZ/XELJANZ XR?
XELJANZ/XELJANZ XR may cause serious side effects, including Hepatitis B or C activation infection in people who carry the virus in their blood. If you are a carrier of the Hepatitis B or C virus (viruses that affect the liver), the virus may become active while you use XELJANZ/XELJANZ XR. Your healthcare provider may do blood tests before you start treatment with XELJANZ/XELJANZ XR and while you are using XELJANZ/XELJANZ XR. Tell your healthcare provider if you have any of the following symptoms of a possible Hepatitis B or C infection: feel very tired, little or no appetite, clay-colored bowel movements, chills, muscle aches, skin rash, skin or eyes look yellow, vomiting, fevers, stomach discomfort, or dark urine.
Common side effects of XELJANZ/XELJANZ XR in rheumatoid arthritis and psoriatic arthritis patients include upper respiratory tract infections (common cold, sinus infections), headache, diarrhea, nasal congestion, sore throat, and runny nose (nasopharyngitis), and high blood pressure (hypertension).
Please see full Prescribing Information including Boxed WARNING and Medication Guide.
PP-XEL-USA-4218
[i] National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). National Institutes of Health, Department of Health and Human Services. Handout on health: rheumatoid arthritis. August 2014. http://www.niams.nih.gov/Health_Info/Rheumatic_Disease/default.asp. Accessed February 14, 2019.
[ii] Hunter TM, Boytsov NN, Zhang X, Schroeder K, Michaud K, Araujo AB. Prevalence of rheumatoid arthritis in the United States adult population in healthcare claims databases, 2004-2014. Rheumatol Int. 2017;37(9):1551-1557.
[iii] Arthritis Foundation. Arthritis by the numbers. https://www.arthritis.org/Documents/Sections/About-Arthritis/arthritis-facts-stats-figures.pdf. Accessed February 14, 2019.