Tri-parish postal centers remain open
February 28, 2012
Terrebonne gains approval of police jurors
February 28, 2012Service cuts to Leonard P. Chabert Medical Center and other facilities in the LSU Health Care System are expected to adversely impact the attracting, training and retaining of young doctors in the Tri-parish region and Louisiana as a whole.
The median level of debt taken on by students attending medical school is $160,000 according to the Association of American Medical Colleges.
Resident doctors training to be physicians and surgeons face a costly future once they commit themselves to learning about and working in the medical field. Understandably, doctors in training want to get the most for their money.
With $34 million in mid-year budget cuts for the LSU Health Care System to officially begin March 5, facilities such as Chabert – its maternity floor and neonatal intensive care unit is scheduled to close Friday as part of $2.9 million in reductions – might not see only the loss of 80 jobs, but could also experience a decline in the number of students wanting to get the most out of their residency program, but not able to do all their work at one location.
Chabert’s residency program is the only one that is fully accredited in the LSU Health Care System, and is one of only seven medical residency programs to have been approved in the United States during the past decade.
“We were accredited in 2008,” Chabert Chief of Medicine Dr. Michael Garcia said. “It is a three year training program with eight class members per year.”
The Houma-based medical facility graduated its first two residents during June 2011.
Garcia said Chabert receives more than 1,100 applications from both inside and outside the U.S. seeking to fill one of eight new spots annually as residency program participants.
Dr. Kevin Leung came from Canada to work on his residency at the Houma facility. He said having the OB/GYN program closed means that not only might future doctors choose to go elsewhere for this part of their training, but current students are left without having a full medical training experience at Chabert.
“With the labor and delivery closed down we won’t be able to rotate here for OB/GYN, which is part of our education,” Leung said. “There is such huge competition by other schools [that cuts] limit the hospitals where we can do it.”
“The goal has been for each training program to plant physicians in the Bayou Region,” Garcia said.
Garcia confirmed studies that claim that more than 50 percent of physicians remain in the regional areas where they train, and maintains that as an objective in his overall efforts. He voiced concern that if the residency programs at Chabert become limited in what is offered, the pool of future physicians for southeast Louisiana could dry up.
In addition to internal medicine and OB/GYN training, Chabert offers patients and young doctors advanced tools in cardiology, dentistry, ophthalmology, vascular and orthopedic surgery and nine other areas of common medical attention.
“The training that is in jeopardy right now is the OB/GYN program,” he said. “The cuts will directly shut down obstetrics at this hospital.”
Medical school graduates decide what specialty area they want to train in, and typically interview at various programs around the country or where they want to go to acquire a residency spot. “These young men and women have selected [Chabert] for their training,” Garcia said. “Part of that curriculum is being eliminated by the state.”
Dr. Bret Hemelt is OB/GYN program director at Chabert. He expressed concern not only for patients and staff, but for those doctors needing to train in this discipline. “[It] is going to be a major change for us,” he said. “[With the cuts] we won’t have as many residents assigned here.”
Garcia explained that it is an intangible number to speculate how many students would choose not to attend the Houma facility because of it no longer offering obstetrics. “We only know anecdotally that when you injure a residency training program it can take as long as 10 years to recover from it,” he said. “So with the state embarking in this cutting of training programs it is really shooting itself in the foot with the creation of its future doctors.”
Current student doctors, like Leung, remain dedicated to continuing in the Chabert residency program, but according to instructing doctors, attracting future residents might become a greater challenge.
“It is a lofty goal to establish a residency program,” Chabert CEO Rhonda Green said. “We are not sure what the final result will be.”
The Chabert medical center is among six public hospitals and science centers in the LSU System to offer educational as well as treatment services. In terms of subject offerings it ranks third with 14 specialty areas for 46 residents. This follows LSU University Hospital in Shreveport with 17 areas of study for 500 residents and Interim LSU Public Hospital in New Orleans with 44 disciplines and 979 residents.
Other LSU System hospitals with medical residency opportunities include Earl K. Long Medical Center in Baton Rouge with 11 programs for 146 residents; University Medical Center in Lafayette with eight programs for 71 residents; E.A. Conway Medical Center, Monroe, 6 programs and 50 residents; Bogalusa Medical Center, Bogalusa, two programs for 15 residents and two programs involving two residents at Lallie Kemp Regional Medical Center in Independence.
Huey P. Long Medical Center in Pineville conducts residency programs in cooperation with Tulane University, LSU Health Science Center in Shreveport, LSU Family Practice in Alexandria and LSU Health Science Center in New Orleans.
The entire LSU Health Care System medical school program is listed as having a total enrollment of 763 first year students and residents, and a total full-time faculty of 565.
Funding for residents in the LSU Health Care System comes through Medicare. Participating hospitals are assigned training slots for residents. The Centers for Medicare and Medicaid send money to training hospitals to pay stipends and benefits for residents.
Additional medical training that could be impacted by the LSU System budget cuts at Chabert includes nursing and medical technician programs from Ochsner Medical Center, Nicholls State University and Fletcher Technical Community College.
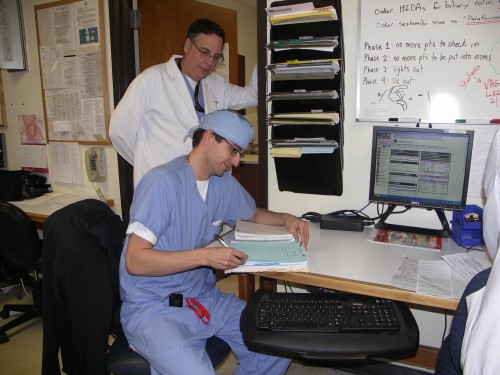
Leonard J. Chabert Medical Center Chief of Surgery Dr. Thomas Weed looks over progress made by medical resident Dr. Jay Luke as part of Luke’s training to become a full-fledged surgeon.